Amazing stuff! Cancer is history (soon)!
Does a daily mouthwash with antiseptics help? We need another study! 😊
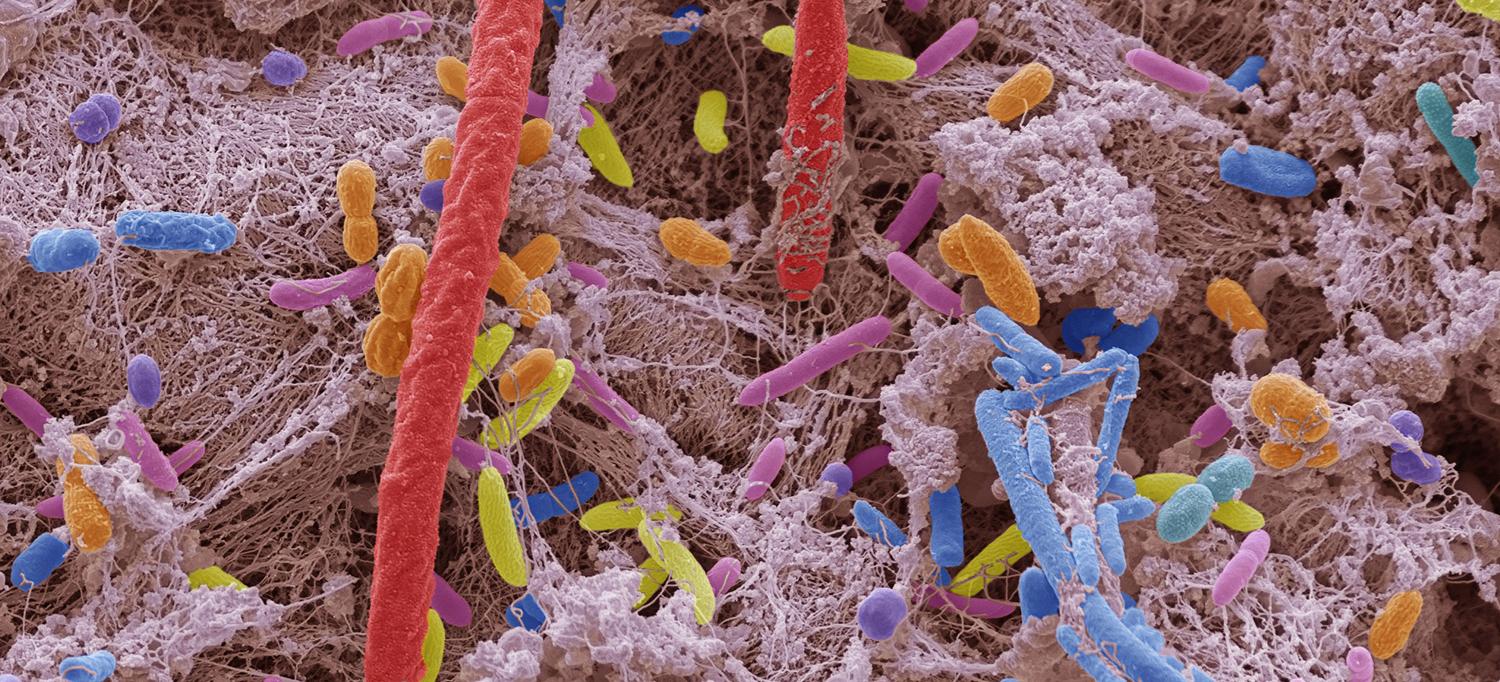
"For the first time, scientists have identified 27 bacteria and fungi living in our mouths that are implicated in the development of pancreatic cancer. Collectively, housing all of the bad microbes increases one’s risk of the deadly disease by 250% – or 3.5 times higher – compared to the general population.
Researchers ... sampled the saliva of 122,000 healthy US men and women, who took part in the American Cancer Society Cancer Prevention Study II and the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial. Samples were collected at baseline, and participants were followed for an average of nine years, with any records of tumors added to the data. ..."
"Among the hundreds of species of bacteria and fungi that live in people’s mouths, 27 have been collectively tied to a 3.5 times greater risk of developing pancreatic cancer ...
Experts have long observed that those with poor oral health are more vulnerable to pancreatic cancer than those with healthier mouths. More recently, scientists have uncovered a mechanism that could help explain this connection, finding that bacteria can travel through swallowed saliva into the pancreas, an organ that helps with digestion. ...
Last year, the same team of scientists uncovered a link between certain oral bacteria and a heightened risk of developing head and neck squamous cell carcinoma, a group of cancers that arise in the mouth and throat.
The researchers had also conducted a small study in 2016 that tied microbes living in the mouth to pancreatic cancer, but could not identify precise bacterial species. ..."
From the key points and abstract:
"Key Points
Question
Is the prediagnostic oral bacterial and fungal microbiome associated with the subsequent development of pancreatic cancer?
Findings
In this cohort study including 122 000 individuals, 3 oral bacterial periodontal pathogens, an additional 20 bacteria, and 4 fungi were identified, which together conferred a more than 3-fold increase in the risk for pancreatic cancer.
Meaning
The oral fungal and bacterial microbiotas may serve as readily accessible, noninvasive biomarkers for subsequent pancreatic cancer risk to identify individuals at high risk of pancreatic cancer.
Abstract
Importance
The oral microbiota may be involved in the development of pancreatic cancer, yet current evidence is largely limited to bacterial 16S amplicon sequencing and small retrospective case-control studies.
Objective
To test whether the oral bacterial and fungal microbiome is associated with the subsequent development of pancreatic cancer.
Design, Setting, and Participants
This cohort study used data from 2 epidemiological cohorts: the American Cancer Society Cancer Prevention Study-II Nutrition Cohort and the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial. Among cohort participants who provided oral samples, those who prospectively developed pancreatic cancer were identified during follow-up.
Control participants who remained free of cancer were selected by 1:1 frequency matching on cohort, 5-year age band, sex, race and ethnicity, and time since oral sample collection.
Data were collected from August 2023 to September 2024, and data were analyzed from August 2023 to January 2025.
Exposures
The oral bacterial and fungal microbiome were characterized via whole-genome shotgun sequencing and internal transcribed spacer (ITS) sequencing, respectively.
The association of periodontal pathogens of the red complex (Treponema denticola, Porphyromonas gingivalis, and Tannerella forsythia) and orange complex (Fusobacterium nucleatum, F periodonticum, Prevotella intermedia, P nigrescens, Parvimonas micra, Eubacterium nodatum, Campylobacter shower, and C gracilis) with pancreatic cancer was tested via logistic regression.
The association of the microbiome-wide bacterial and fungal taxa with pancreatic cancer was assessed by Analysis of Compositions of Microbiomes With Bias Correction 2 (ANCOM-BC2).
Microbial risk scores (MRS) for pancreatic cancer were calculated from the risk-associated bacterial and fungal species.
Main Outcomes and Measures
Pancreatic cancer incidence.
Results
Of 122 000 cohort participants who provided samples, 445 developed pancreatic cancer over a median (IQR) follow-up of 8.8 (4.9-13.4) years and were matched with 445 controls.
Of these 890 participants, 474 (53.3%) were male, and the mean (SD) age was 67.2 (7.5) years.
Three oral bacterial periodontal pathogens—P gingivalis, E nodatum, and P micra—were associated with increased risk of pancreatic cancer.
A bacteriome-wide scan revealed 8 oral bacteria associated with decreased and 13 oral bacteria associated with increased risk of pancreatic cancer (false discovery rate–adjusted Q statistic less than .05).
Of the fungi, genus Candida was associated with increased risk of pancreatic cancer.
The MRS, based on 27 oral species, was associated with an increase in pancreatic cancer risk (multivariate odds ratio per 1-SD increase in MRS, 3.44; 95% CI, 2.63-4.51).
Conclusions and Relevance
In this cohort study, oral bacteria and fungi were significant risk factors for pancreatic cancer development. Oral microbiota hold promise as biomarkers to identify individuals at high risk of pancreatic cancer, potentially contributing to personalized prevention."
No comments:
Post a Comment